Organs located in a bone roof in the genital region can move in a limited manner due to various bonds that fasten them. These bonds might lose their edge with increasing age and especially as the number of deliveries increase and might lead to the prolapse of genital organs into the vagina.
Genital prolapse is the name given to the migration of the uterus, bladder and pelvic colon downwards in the vagina.
Sometimes the prolapse is so apparent that the woman can feel her cervix in the entrance to her vagina by hand (desensus uteri). The uterus might sometimes prolapse completely (total prolapse).
Bladder prolapse (cystocele) is the name given to the bulging of the bladder which is adjacent to the front wall of the vagina. This condition makes women feel the bladder bulging within the vagina by hand under situations such as coughing, sneezing, lifting a heavy object that increase intraabdominal pressure.
Rectum (large intestine) prolapse (rectocele), on the other hand, is the bulging of the rectum, which is adjacent to the posterior wall of the vagina, towards the vagina.

Incidence of the disease
Prolapse in genital organs is observed especially in women who has been through a large number of difficult deliveries. Protracted deliveries result in elongation of bonds keeping genital organs in place, laceration thereof in some regions and thus a reduction in the capacity to keep the organs in place.
Prolapse is less often seen in women who had cesarian section or women who have not given to any children at all.

What Symptoms Does It Have?
When uterus prolapse occurs by itself, it causes a woman to feel pain and fullness in the lower region especially when she is standing up, coughs, sneezes and strains. In advanced stages of the disease, the prolapse results in the uterus’s protruding from the vagina as a whole. In this case, which is observed relatively rarely, the organs protrude again even after the woman pushes the organs back into her vagina with her fingers.
Bladder prolapse causes the angle that must exist between the bladder and the pipe called urethra, which transfers urine from the bladder to the external environment, to disrupt, thus leading to urinary incontinence in advanced stages of the disease.
In its mildest form, urinary incontinence occurs while coughing only. When the severity of the prolapse increases, urinary incontinence starts appearing in such conditions as laughing, standing as well. In the most severe and quite rare cases, urine cannot be held at all and the urine reaching the bladder is directly discharged without being stored.
Although rectum prolapse does not lead to special problems in many cases, it might cause constipation in some cases.
Another problem experienced by women having prolapsing genital organs is the enlargement of the entrance to the vagina by tears resulting from dystocia. This might cause the woman to have problems in her sexual life with her spouse.
Genital organ prolapses are rarely seen singly. They are usually accompanied by uterus prolapse, bladder prolapse and rectum prolapse.

How is a diagnosis made?
Genital organ prolapse is often diagnosed when the prolapse is seen during the gynecological examination of a woman experiencing urinary incontinence or “fullness in the lower region”. It might also be detected by chance in a women who has no problems at all.

How is it treated?
If a woman, who has completed her family, suffers from genital organ prolapse, the treatment to be administered will usually be to remove the uterus from the vaginal route and to remove the excesses on the anterior and posterior walls of the vagina. Administration of different method of surgery might be required to treat urinary incontinence.
However, if a woman, who is young and thinking of giving birth to children, suffers from genital organ prolapse, the excesses on the anterior and posterior walls of the vagina might be removed without removing the uterus. In case of an apparent uterus prolapse, bonds keeping the uterus in place might be accessed through the abdomen and pushed upwards.
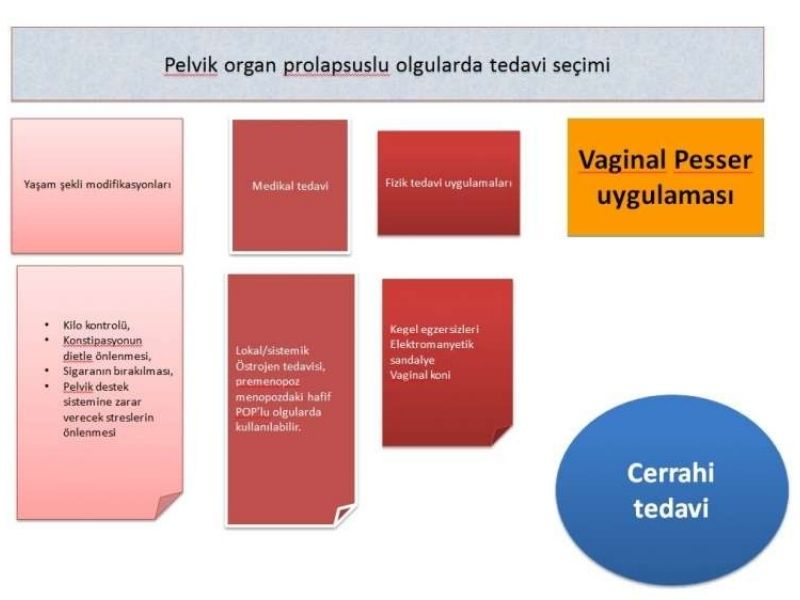
Selection of Treatment In Cases with Pelvic Organ Prolapse
Yaşam şekli modifikasyonları: Lifestyle modifications
Medikal tedavi: medical treatment
Fizik tedavi uygulamaları: Physical rehabilitation practices
Vaginal Pesser Uygulaması: Vaginal Pessary Implementation
Kilo kontrolü: weight control
Konstipasyonun diyetle önlenmesi: Prevention of constipation via diet
Sigaranın bırakılması:Stopping smoking
Pelvik destek sistemine zarar verecek streslerin önlenmesi: Avoidance of stress that might give damage to the pelvic support system
Lokal/sistemik östrojen tedavisi, premenopoz/menopozdaki hafif POP’lu olgularda kullanılabilir: Local/systemic estrogen treatment can be administered in cases with mild POP who are in the premenopausal period or menopause.
Kegel Egzersizleri: Kegel Exercises
Elektromanyetik sandalye: Electromagnetic chair
Vaginal koni: Vaginal cone
Vajinal Pesser Uygulaması: Vaginal Pessary Practice
Cerrahi Tedavi: Surgical Treatment
A: RING
B: SHATZ
C, D,F: GELHORN
E: REINFORCED RING
G: RİSSER
H: SMITH
I: TANDEM CUBE
J: CUBE
K: KNOBBED HODGE
M: GEHRUNG
N: REINFORCED INCONTINENCE PLATE
O: DONUT
P: INCONTINENCE RING
Q: INCONTINENCE PLATE
R: REINFORCED HODGE
S: INFLATOBALL

- A nonsurgical alternative in the treatment of POP.
- Pessary runs the risk of falling or causing irritation
- Might be adversely affected by sexual intercourse
- Needs to be removed and cleaned regularly.
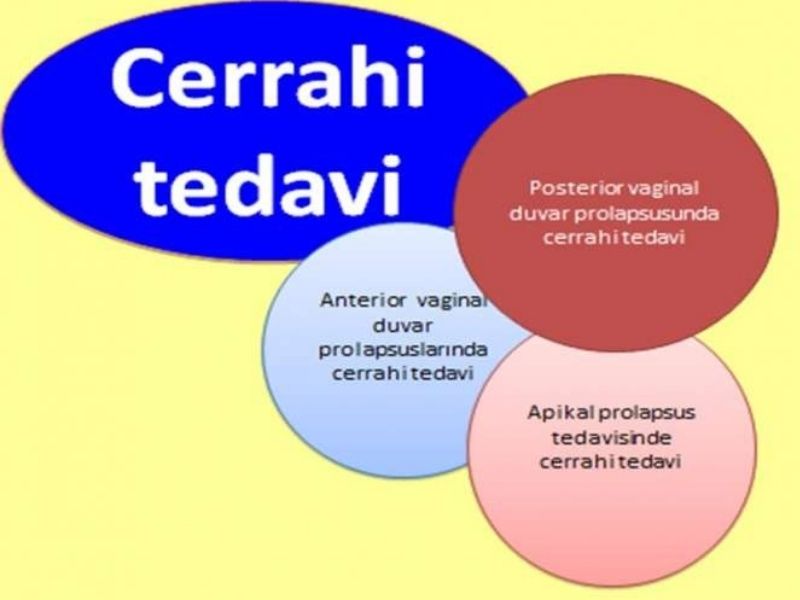


Cerrahi Tedavi: Surgical Treatment
Surgical Treatment of Anterior Vaginal Wall Prolapses
Surgical Treatment of Posterior Vaginal Wall Prolapses
Surgical Treatment of Apical Genital Prolapses
Sacrocolpopexy
- 85-100% success achieved in anatomic correction
- 74-91% success achieved throughout 14-year monitoring
Abd Skp vs Vaginal SSF
- Skp operations are more successful
- Failure observed earlier in the SSF group
In Skp Operations
- Bladder, ureter, intestine injury reported apart from per-operative complications
- Mesh erosion reported
Apical (midline) Prolapse Surgery
Reconstructive
Abdominally Vaginally
Sacrocolpopexy Sacrospinous fixation operation
Sacrocervicopexy Iliococcygeal fixation operation (prespinous fixation)
(open-L/S) McCall Culdoplasty
Posterior intravaginal slingplasty (Posterior IVS)
Whereas the vaginal method in reconstructive surgery provides advantages such as faster recovery and shorter durations of surgery,
the abdominal method
Approach to additional intraabdominal pathologies
Operation of cases with short vaginal stumps
Obliterative
Colpocleisis
Comes to the foreground as a minimal invasive operation for elderly women who are not sexually active.
Posterior Vaginal Compartment
-
Rectovaginal facial defect, loss of support by the levator ani muscle and raised rectovaginal pressure shift play a role in the pathogenesis of posterior compartment pathologies.
-
Annual incidence of rectocele is known to be 5.7/100 women.
Treatment
Whereas the transanal or abdominal methods are preferred in cases with rectal mucosa prolapse and intussusception in rectocele treatment, treatment is administered transvaginally ** in cases with rectocele other than those above.
There are studies reporting 18-20 relapse after colporraphy posterior facial repair.
Mesh Surgery
100% success has been reported in a follow-up of 60 months. However, mesh erosion rising up to 12% is reported in studies











METE İTİL
Appointment and Contact Form
You can ask us your questions or contact us to make an appointment.